|
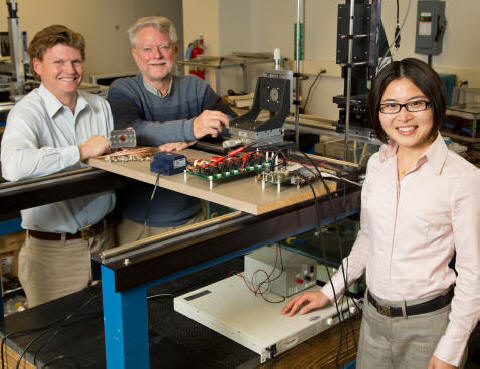
L to R: Gabe Owens, MD, Ph.D.,
Charles Cain, Ph.D., and Zhen Xu, Ph.D., The University
of Michigan
"Knifeless" Surgery for the Treatment of Congenital
Heart Defects
Memphis, TN, October 05, 2012 -- The Hartwell Foundation officially announced today a grant to three researchers at The University of Michigan: Charles Cain, Ph.D., 2007 Hartwell Investigator and Professor of Biomedical Engineering, Gabe Owens, M.D., Ph.D., Assistant Professor of Pediatric Cardiology and Zhen Xu, Ph.D., Assistant Professor of Biomedical Engineering for Pediatric Histotripsy, Ultrasound-mediated “Knifeless”- Surgery for the Treatment of Congenital Heart Defects: Preparing for a Clinical Trial. The researchers will seek requisite preclinical safety and functionality data in preparation for a small human clinical trial on infants with hypoplastic left heart syndrome (HLHS). Over three years, the trio will receive $884,165 in direct costs from the Foundation and matching funds from the University. The University of Michigan is a Hartwell Foundation Top Ten Center of Biomedical Research.
Pressure caused by blood-flow to each chamber of the heart is believed to produce the primary stimulus for normal development of the fetal heart. In HLHS however, normal blood flow during fetal development is obstructed, resulting in a poorly functioning and underdeveloped left ventricle (or pumping chamber). The valves on the left side of the heart (aortic valve and mitral valve) also don't work properly, and the main artery leaving the heart (aorta) is smaller than normal. After birth, oxygenated blood from the lungs cannot be pumped out of the heart by the small, underdeveloped left ventricle and through the aortic valve to the rest of the infant's body.
HLHS is the most common severe congenital heart malformation, with about 1000 new cases each year in the US; the cause is unknown. There is no cure and a 3 stage surgical reconstruction and reconfiguration of the major blood vessels must be initiated so the heart can function with only one ventricle. While the first surgery begins a few days after birth, the last stage of surgery does not occur until 18-36 months. Without surgical intervention, the HLHS defect is uniformly lethal. Nonetheless, even following successful surgery the prognosis for vibrant long-term health of the affected child is poor, with mortality at 35-40%.
In theory, correcting abnormal blood flow in the HLHS heart early in pregnancy, during fetal development, should encourage proper growth of a heart with two functioning ventricles. A surgical approach to physically create a channel to alter blood flow through the left side of the heart while the fetus is still inside the uterus (in utero) could be used, but it would pose significant risk to both the fetus and the mother. Such invasive surgery in utero requires cutting through the mother’s abdomen to gain access to the uterus and fetus, and then cutting through the fetal skin and heart; a procedure that carries a high risk of inducing preterm labor, infection, and fetal death. Another, less invasive alternative that has demonstrated technical feasibility involves catheterization of the mother in order to secure access to the fetal heart. While somewhat less invasive than a direct surgical approach, cardiac catheterization of the fetus in utero to precisely create a channel between the two ventricles is difficult to perform and accurately control. By contrast, surgical intervention after birth may be safer, but it can not correct the HLHS defect and is only a palliation.
Charles Cain developed the required technologies to establish a proof-of-principle for "knifeless surgery" intended for pediatric cardiac applications with funding from a 2007 Hartwell Individual Biomedical Research Award. The approach was based upon his ultrasound innovation he called histotripsy, which works by generating acoustically formed bubbles within tissue from a non-invasive probe that rests outside of the body. The cloud of extremely small bubbles act as "mini-scalpels" to precisely create a channel only at the treatment focus; without bleeding, stitches, or risk of infection. Hypothetically, a channel created in this way between the ventricles of an abnormal heart would permit blood flow in early fetal development to effectively redirect the growth of heart tissue so that HLHS never fully occurs. Unfortunately, there are no appropriate animal models for the syndrome to confirm the validity of this hypothesis.
It has only been possible to demonstrate the feasibility of histotripsy intervention by non-invasively creating channels in otherwise normal animal hearts in utero. Cain, Owens and Xu have already acquired preliminary data to show how flow channels can be created non-invasively between chambers within the beating heart of both an adult dog and a newborn pig, as well as in a fetal sheep heart in utero. Although still at an early stage, there is compelling evidence for the effectiveness of their technology and no evident safety concerns, as confirmed by the absence of peripheral tissue damage. A clinical trial is anticipated by the end of the third year of the Hartwell grant.
The Hartwell Foundation seeks to inspire innovation and achievement by providing financial support to Hartwell Investigators to jump start the clinical translation of transformative biomedical research that can potentially benefit children.
"Support for clinical translation of this innovation was possible because matching funds were available from other university sources and sufficient infrastructure exists within The University of Michigan to sustain an eventual clinical trial," said Fred Dombrose, President of the Hartwell Foundation.
|
|
Top Ten Centers
Individual Biomedical
Research Awards
|

